Make Running A Salon Easier With The All-In-One Salon Management System,



5 Salons in Leicestershire
Spring 2012
EVERYTHING…especially SMS and Email Marketing
For Barrie, the ability to access his business on the cloud from all around the world was key when selecting a salon software provider.
SalonIQ also enables the teams to stay agile, reactive and focused through KPIs, team reporting and IQ’s client engagement tools.
1 Salon in the beautiful town of Quorn
Summer 2016
Marketing, Reports and being able to access SalonIQ from ANYWHERE
Not being happy with their previous software provider, Mags made the switch to SalonIQ and it was “the best thing they did”. The move was stress free and they now feel fully supported as a business.
Stones hair describe SalonIQ as “Affordable, Reliable and Always Evolving”.
30+ Salons in Central & Southern England
Autumn 2020
Dashboards and online bookings
Francesco Group were looking for a forward thinking software partner that would work closely with their business. Having access to their business 24/7 from anywhere is vital to the team at Francesco Group. The intelligent marketing within SalonIQ also helps to drive their business forward.
9 Salons in Central England
Spring 2012
Dashboards and online bookings
Harry was feeling fed up with his previous salon software so reached out to David for a chat…the rest they say is history.
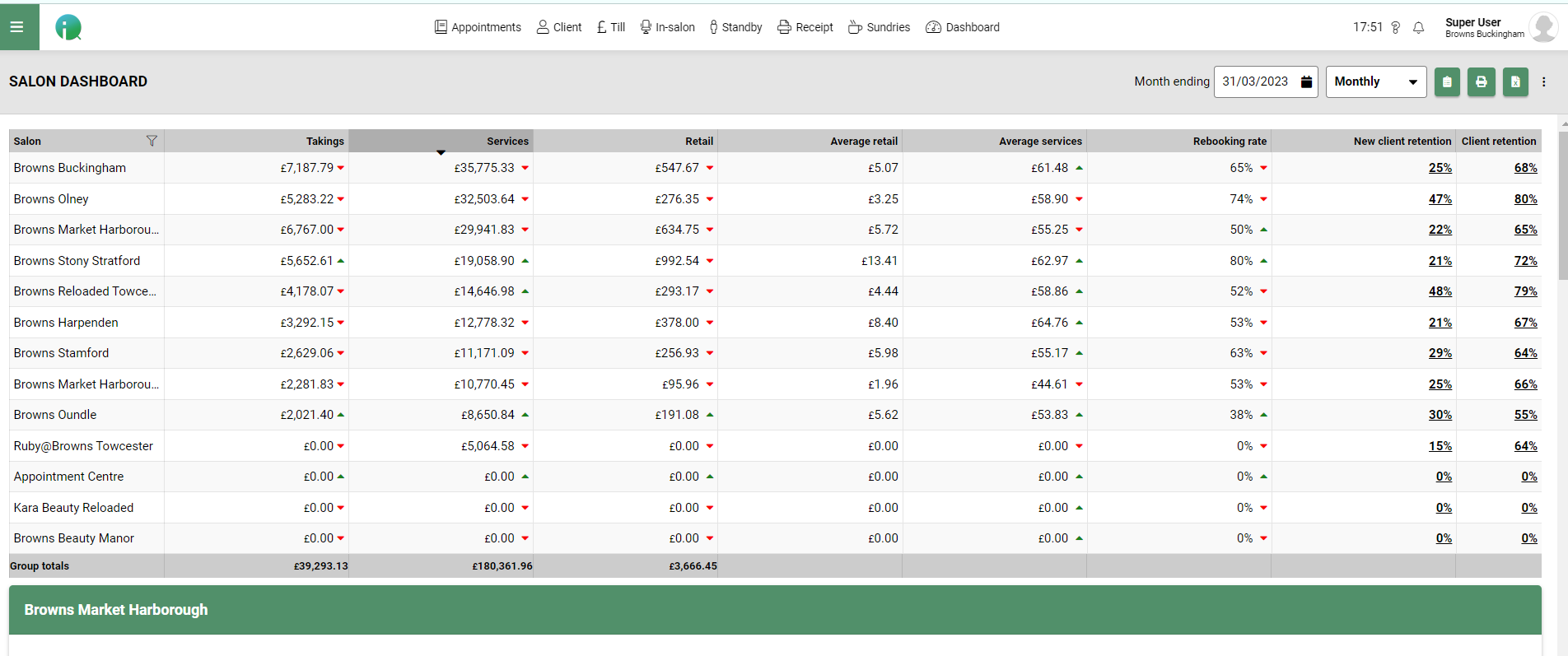
Browns Hairdressing constantly boost their growth using SalonIQ – attracting new clients, attending our regular online masterclasses and following our marketing campaigns.
7 Salons across Derbyshire
Autumn 2018
ALL of the reports and the daily business stats.
Sally has been using SalonIQ in all of her salons for over 5 years and is loving it, she could not live without the detailed end-of-day reporting, plus the ability to be able to access and view all of her salons anywhere in the world. Sally also loves that she can interact with her team and clients using the system any day, any time.
1 Salon in Telford
Summer 2018
SalonIQ reports and marketing hub
Kayleigh was recommended to SalonIQ by a fellow salon owner. Having her client data safe and all in one place has saved so much admin time so she can spend more time focusing on her clients.
2 Salons in Telford & Shrewsbury
Summer 2018
DATA…Reports, figures and did we say reports?
After researching software in depth, Debbie made the move to SalonIQ as the software ticked all of the boxes for her business.
Debbie also makes the most from the marketing hub and our FREE unlimited training to help grow her team and business.
2 Salons in Leicestershire
Autumn 2022
Online bookings and their bespoke client app
Stephanie wanted more remote access using a cloud-based system and knew SalonIQ was right for what she needed.
Stephanie was worried about switching, but shares how easy and simple the switching process was and how she feels so supported by the IQ team.
1 Salon in Sutton Coldfield
Summer 2022
Online bookings and Aveda Benchmark report
After using another software provider, Angela just knew there were better providers out there…And then she was told about SalonIQ.
Angela can now manage her team fully with easy access to targets and KPIs.
1 Salon in Sutton Coldfield
Autumn 2020
SMS reminders which have reduced no-shows to zero.
Ian McCloud switched from another provider to SalonIQ as he wanted to work with a forward thinking company and have easy access to his business whenever he liked.
Being able to see the Return on Investment from the marketing generated is a favourite for Ian and his team.
Highly successful, award-winning 5 salon group in Surrey. SalonIQ has helped streamline their operations, Enhanced their marketing, and put their owner Salv firmly in control of the entire estate.
Sean Hanna is one of the UK’s leading hair salon groups. Born in Worcester Park in 1981, the brand has won hundreds of awards, including Salon Group of the Year (Fellowship of British hairdressing)and the very prestigious London Hairdresser of the year (The British Hairdressing Awards. Sean Hanna has 6 salons based in London and Cambridge. The owner’s Sean and Skyler, are highly passionate about their team and clients. SalonIQ provides complete visibility across the group.
Leanne has had SalonIQ software in her salon since the day it all started and could not be without it now.
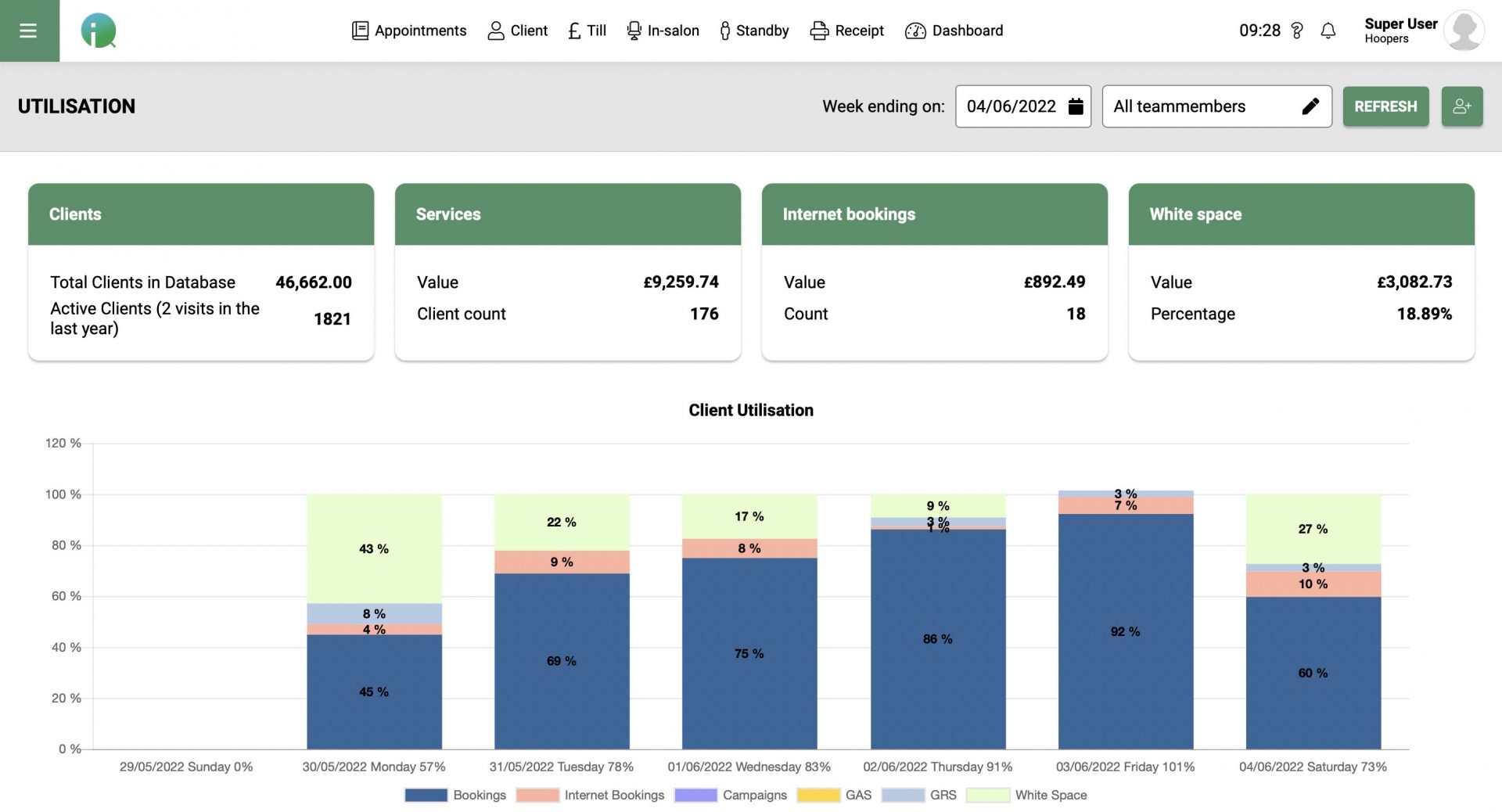
The dashboards are something Leanne goes to all the time to get a real overview of how her salon is performing, it is laid out in such a way that it is simple and easy to read if you are short on time.
Leanne uses the SMS alerts as well as the email confirmations every single day. It is a great way to make contact with clients that have been booked in for some time to ensure they can still make their appointment.
SalonIQ has been a revolution for Paul’s salon business since changing over from his previous salon software. One of the areas flagged up for Paul since the transition was noticing the amount of promotions and offers they were doing as a salon business. As they have now become aware of this they have now reduced the amount of promotions that they offer at any one time.
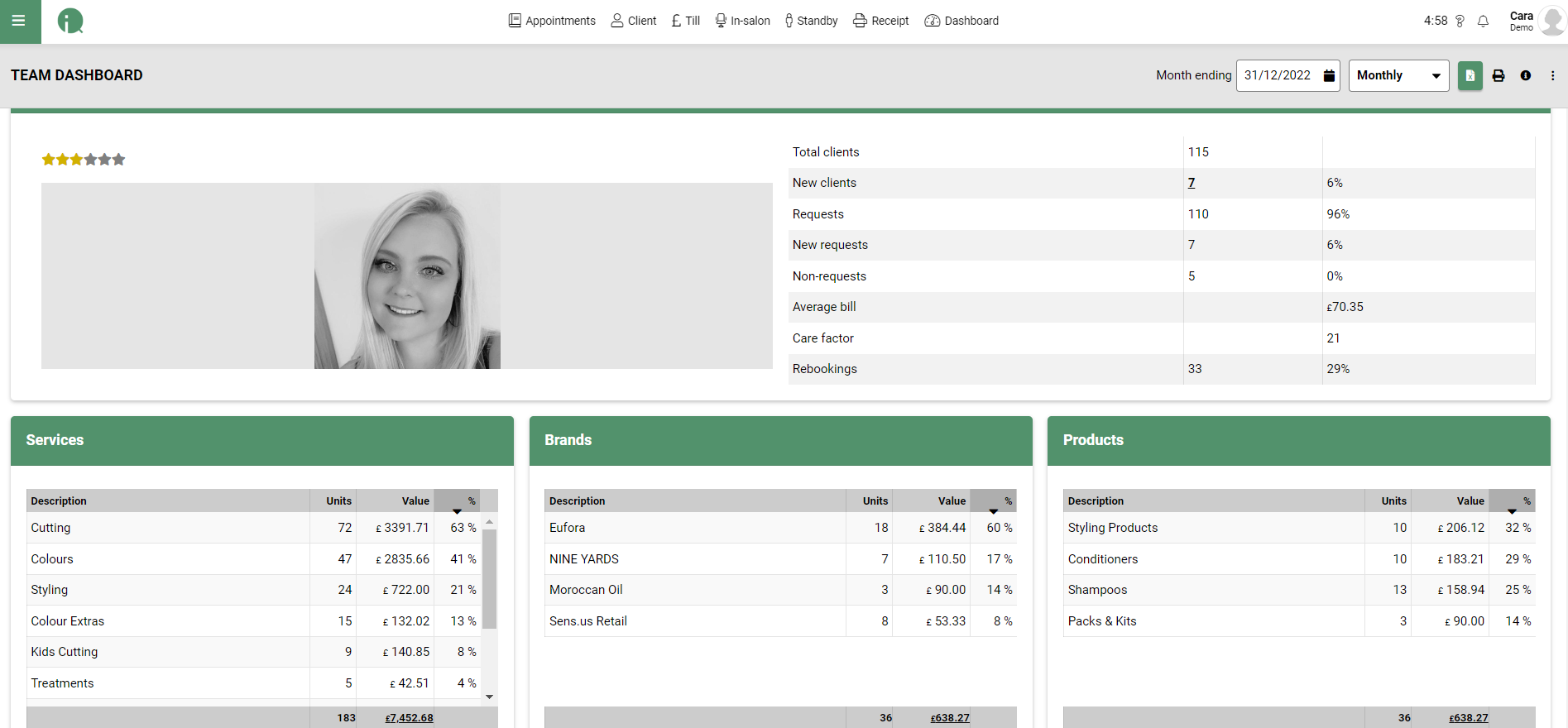
Another key area that is used a lot by Paul and his team members are the dashboards, both the team and salon dashboards. These are looked at on a daily basis to help show performance and areas for improvement through out the days and weeks.
Zappas are a group of 6 salons in the Berkshire, Hampshire area. Steve employs around 150 staff so having full visibility of the day to day running of each salon is key.
Steve is now able to see exactly what is going on in each salon where ever he is at home work or away. Steve particularly likes the dashboards as he is able to make quick comparisons for services, retail and salon performance.
Karine Jackson owner of Karine Jackson Salon in the Westend and President of Fellowship has been with SalonIQ now for 2/3 years. Karine loves how Salon IQ software sends out automated messages to team members at the end of each day and week to inform them of their performance. They now depend on it.
Karine found that no shows were a bit of a problem in her salon, so has now introduced deposits with online bookings via SalonIQ, which enables the clients to pay upfront.
Karine also likes how we work along side her salon business, continuously listening to what Salon business needs are and developing the software accordingly.
Charlie Miller joined SalonIQ at the end of 2017. One of the great things Charlie Miller loved from the very beginning was the smooth and easy transition of moving the salon data and all future appointments across from their old salon software to Salon IQ software.
The fact that SalonIQ is cloud based is the way forward for salon software. When SalonIQ send out a new release with all the latest updates you do not need to do a thing as the software does it all for you. No backups are needed for each device you use as it is all there for you.


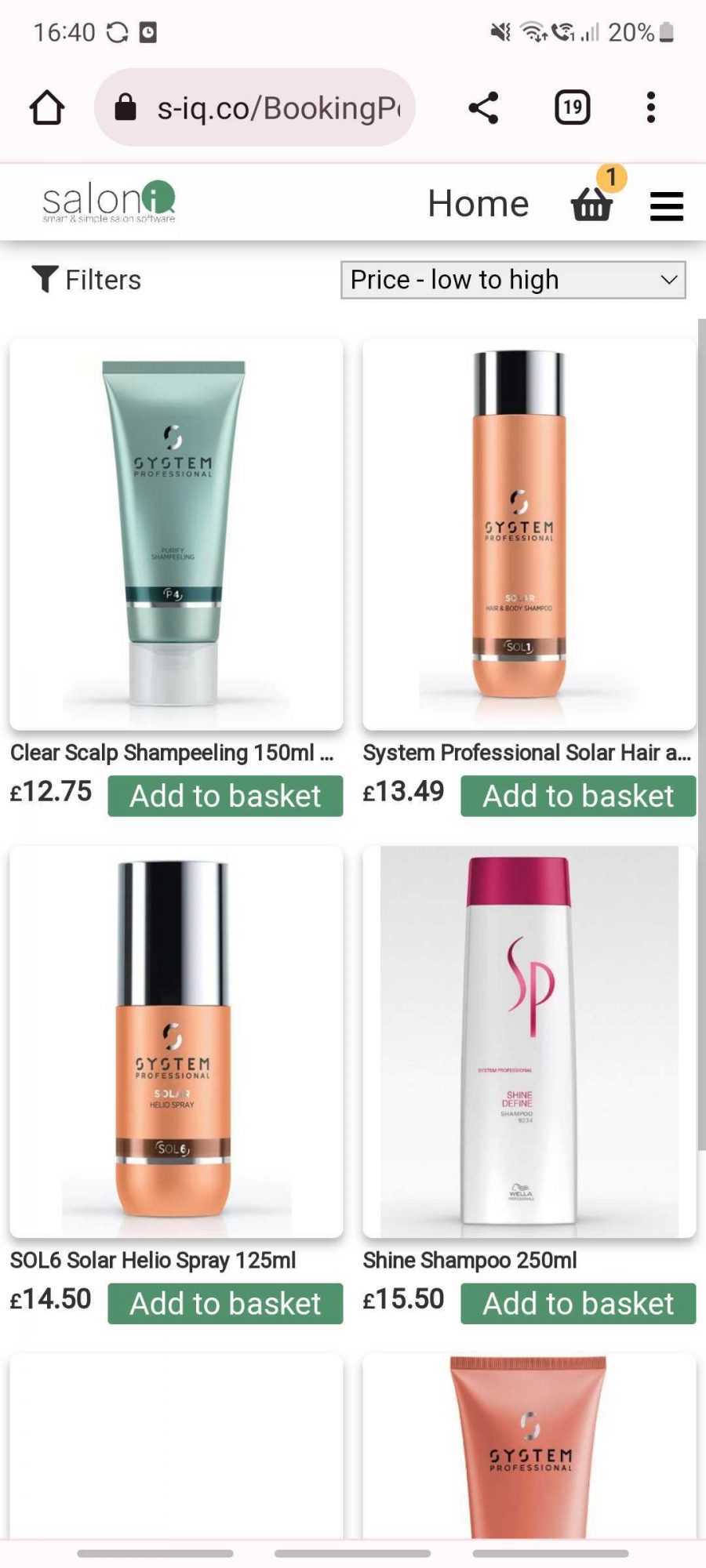
Online Booking 24x7 Elevating your client Experience.
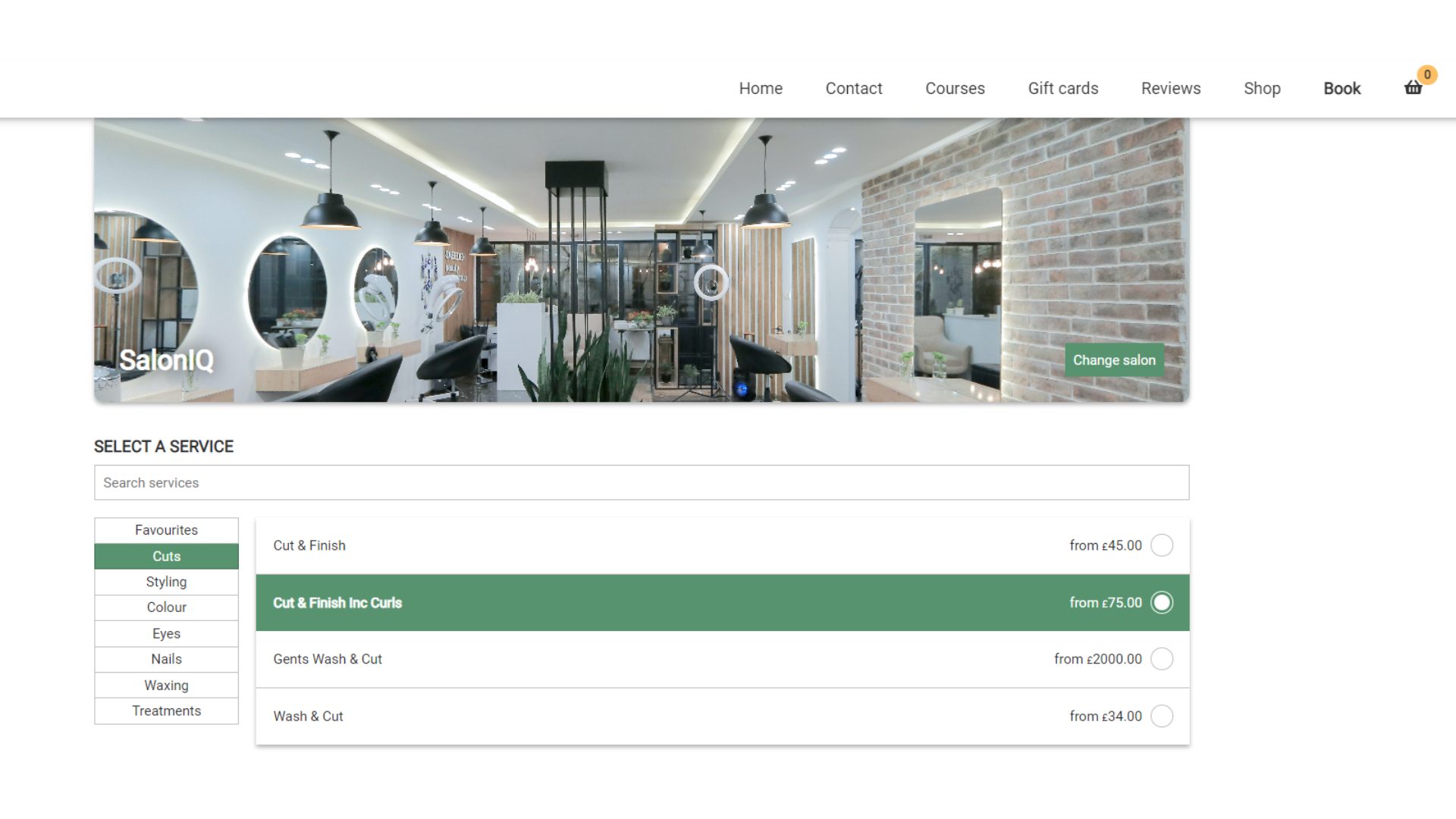
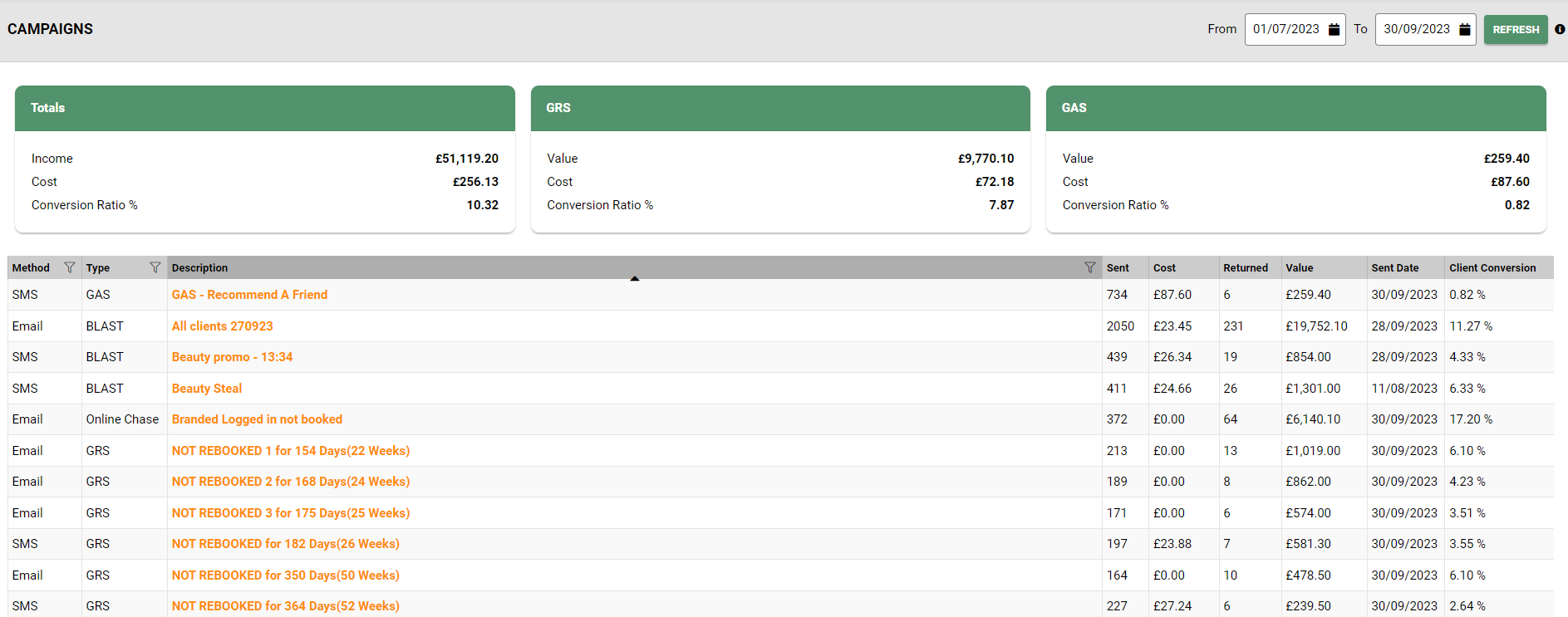
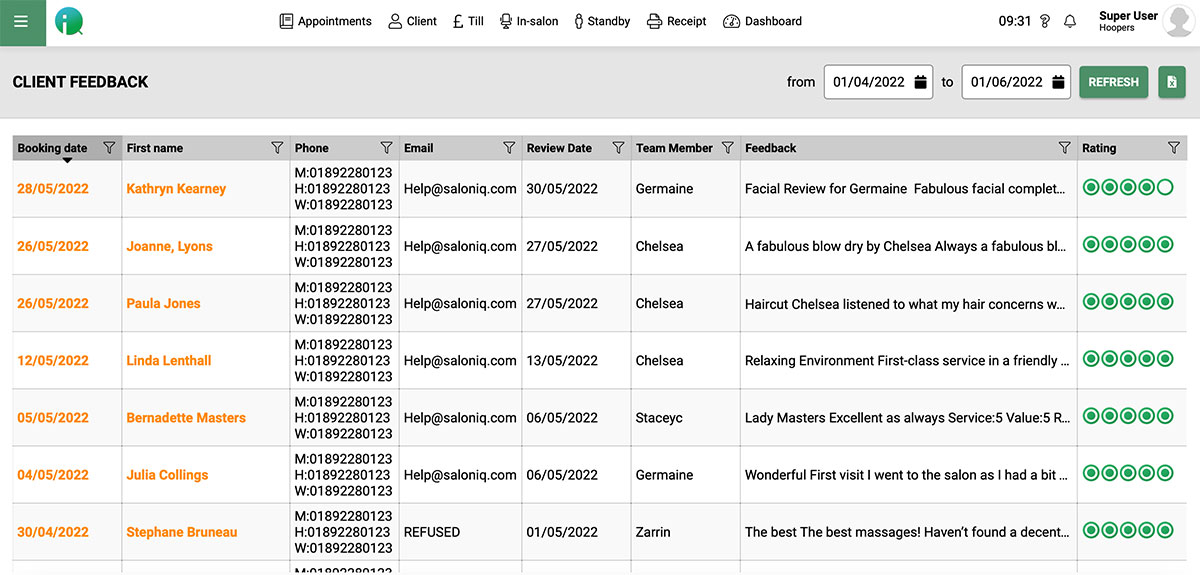
Master your marketing with SalonIQ's marketing strategies and promotions
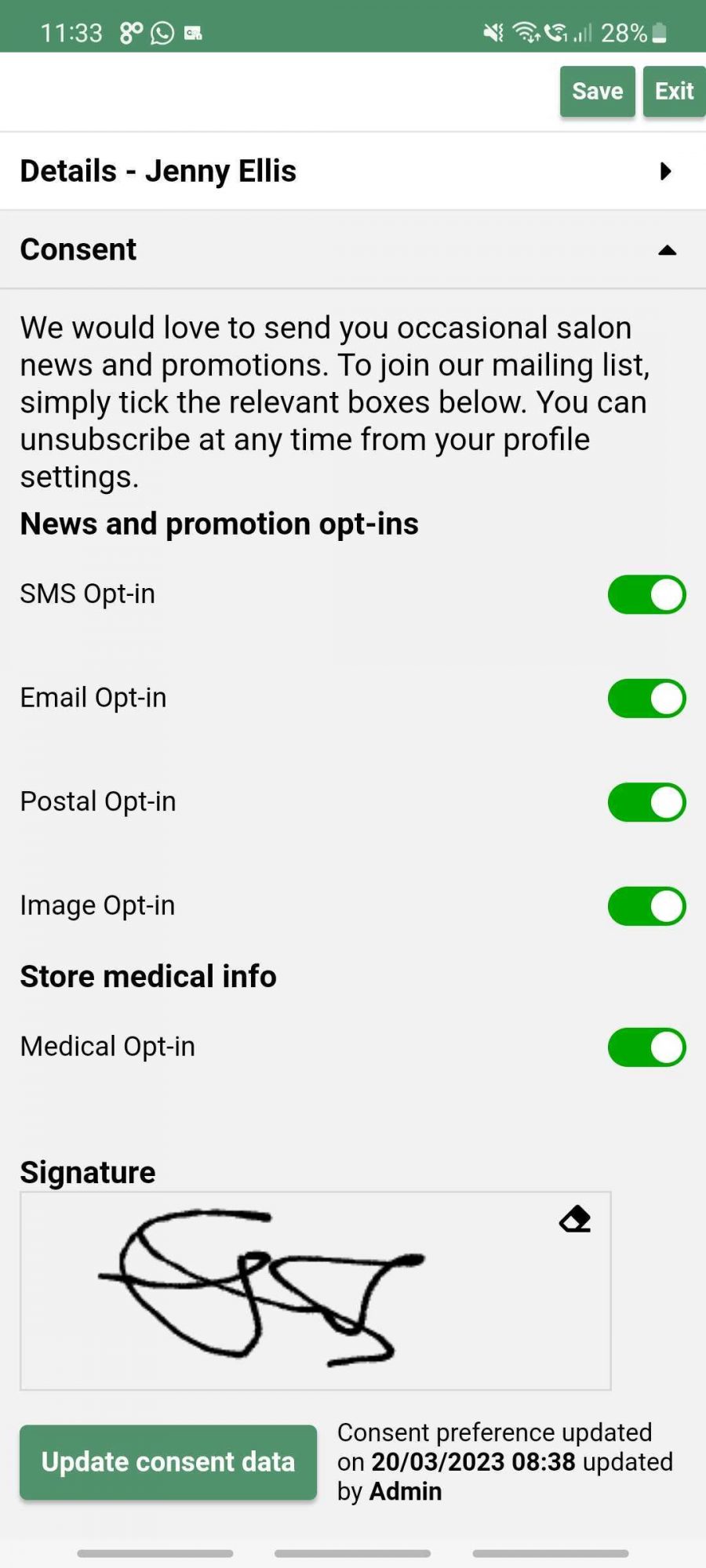
Take Deposits, Client Intake, Client Payments, Follow up marketing and re-bookings.
Motivate your team, monitor performance and stay on top of your team.
Salon Software Designed and built For Enterprise. Multisite software that grows with you.
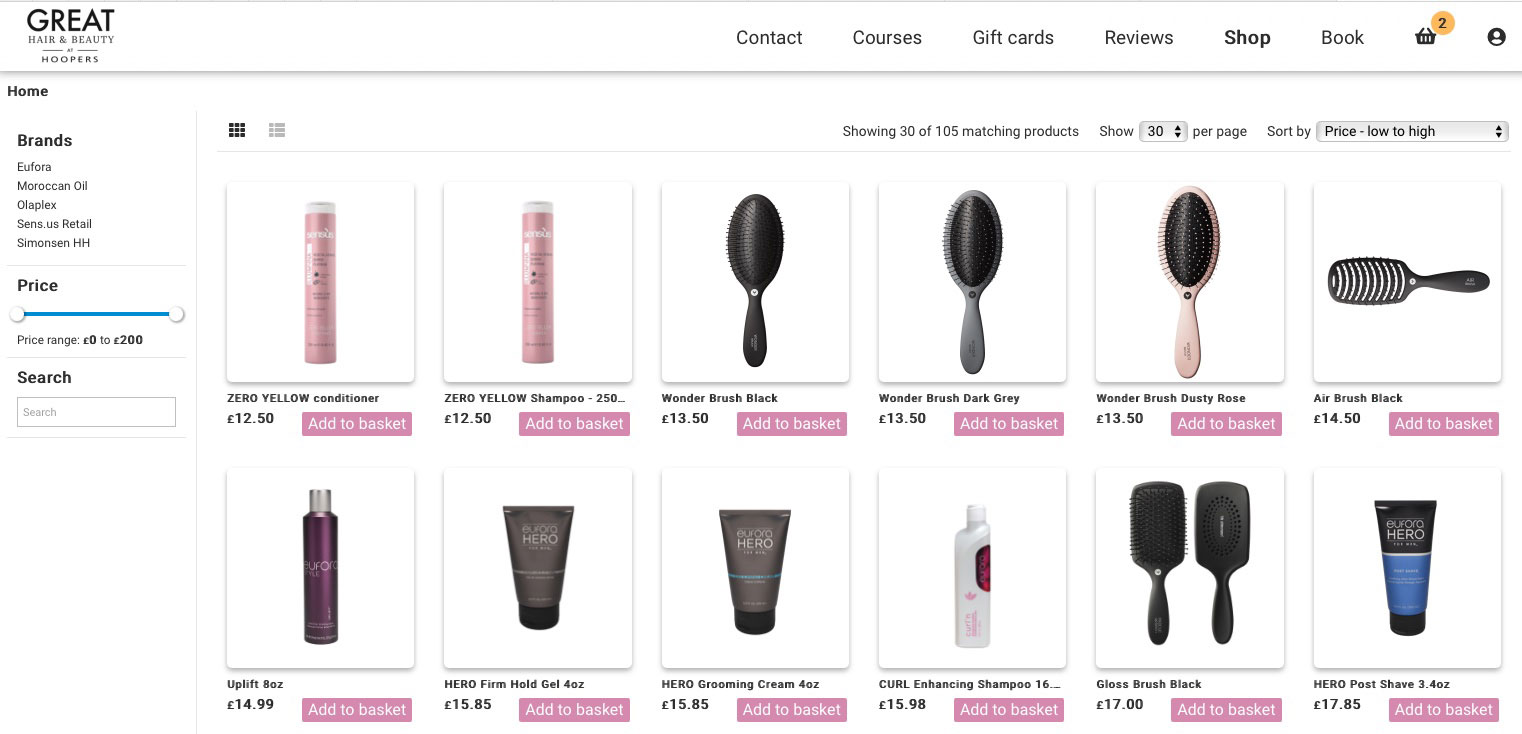
Maximise your salons retail potential with our recommendation system.
Make Running A Salon Easier With The All-In-One Salon Management System,
Take your business to new heights with our simple, flexible and powerful booking software.
Salon IQ has revolutionised the way we run our salon.
4.8

of Bookings made online
ROI new client referrals
lost client reactivation
reduction of no shows
Read our Verified Google Reviews
"Extremely pleased with SalonIQ both for the salon software and for the support received so far. Just had another training session today with Kate and she was very kind and helpful, with great recommendations on how to use it. Recommended!"
LUIGI BISBIGLIA April 2024
"I have had 2 meeting with Jessica now and she is just fantastic. Real helpful with any questions i have. Is super easy to get in touch with as well on emails. Jessica is just an all round lovely lady. Look forward to our next meeting and creating new ideas together x"
Daniel Granger Hairdressing March 2024
"Just had a fantastic 1 hour review meeting with the lovely Kate. She was like a breath of fresh air & managed to cram so much into our 1st hour, with plans for next time to boot! You have left us all buzzing with a new enthusiasm for the future. Thankyou so much - Nick & Team Bliss xx"
Nick Tedd November 2023
"Jessica has been helping set up my CRM system for my newly opening business and wow she is amazing! She works non stop at all hours to get things done for us, she’s always there to help whenever I have any questions. So impressed with the customer service 🥰"
Sidrah Hussain April 2024
"Using SalonIQ as a CRM for an Aesthetics clinic. We are 2 months in and so far it is excellent. Super easy to use, really good marketing functionality and the level of customer support is really impressive."
Carl Gillespie April 2024
Users
SMS Sent
Annual Bookings
Transactions/year




Call a member of our team today on 01892 280 123